
When you notice curare clefts in your capnography waveform, you only have 2-3 minutes to re-administer the neuromuscular blockade before the patient comes out of paralysis.ĭuring cardiopulmonary resuscitation, waveform capnography can serve a variety of valuable functions. If the baseline is above zero in a mechanically ventilated patient and the Beta angle is greater than 90 degrees, this is an indication that the patient is rebreathing carbon dioxide. Pay particular attention to the inspiratory baseline (Phase 1) in mechanically ventilated patients.

When documenting a change in ventilator rate settings and why, be sure to include PaCO2 and PetCO2 and the time each was measured (ideally, within the same time frame), and the change in PetCO2 with the new settings.

If the end-tidal gradient, P(a-et)CO2 is more than 10 mm Hg, a shunt exists, but it is impossible to determine this unless you are comparing capnography readings and arterial blood gases measured within the same time frame. If the patient has significant ventilation/perfusion (V/Q) mismatch due to pulmonary shunting, you risk hypoventilating the patient when titrating ventilations to PetCO2. Use caution in changing ventilator rate settings to titrate ventilations to a normal PetCO2 reading. However, most intubated patients do not have normal pulmonary physiology, or they wouldn’t have been intubated in the first place. Normal PaCO2 is 35-45 mm Hg, therefore PetCO2 would theoretically be 34-44 mm Hg, and should never be more than 5 mm Hg less than the arterial CO2 in patients with normal pulmonary physiology. Document initial PetCO2 readings, and compare those to arterial blood gases, if any are available. In patients with normal pulmonary physiology, end-tidal carbon dioxide (PetCO2) should be no more than 2-5 mm Hg less than arterial carbon dioxide (PaCO2), and is usually within 1 mm Hg of PaCO2. When attaching a capnograph to an intubated, mechanically ventilated patient, there are four parameters to consider: initial ETCO2 reading, waveform morphology, ventilatory rate, and respiratory baseline (Phase I) measurement. Just like with normal breathing, ventilatory rate in mechanically ventilated patients has a direct bearing on ETCO2.
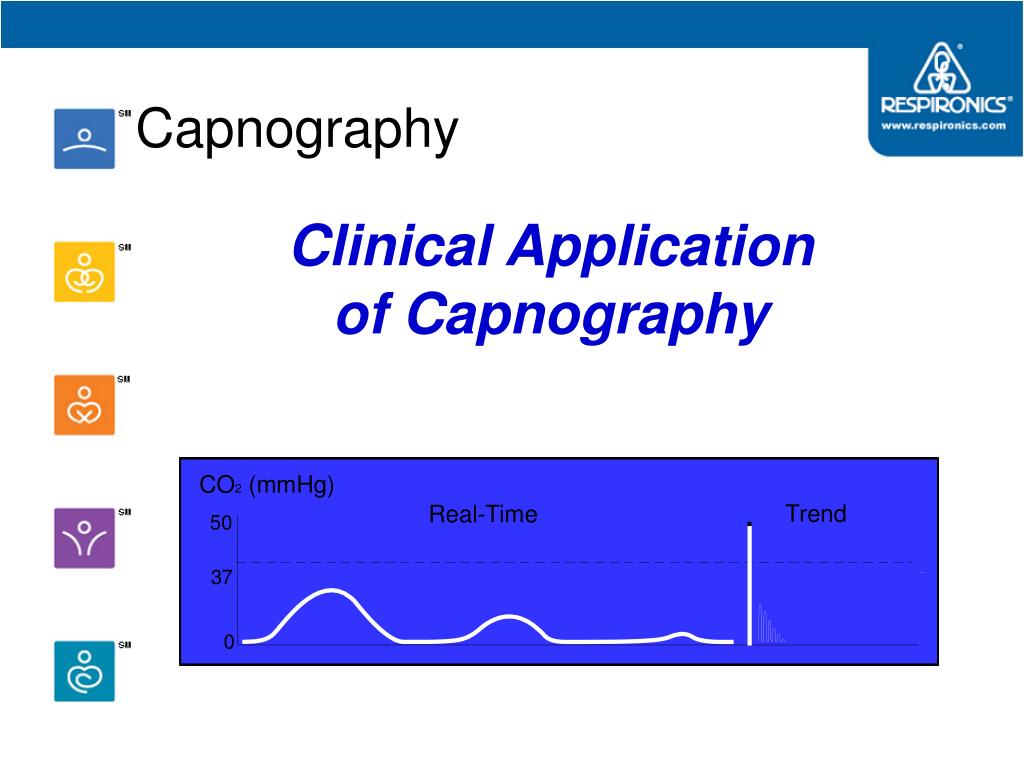
Intubated and mechanically ventilated patients Simply put, we should be using capnography on any patient with significantly decreased level of consciousness, or any significant derangement in oxygenation, ventilation, or perfusion. When we understand that capnography is the only real-time measure of the effectiveness of ventilation and a reliable indirect measure of perfusion, then that opens up an entire new world of applications. There is an old medical truism that states, "If you never check a temperature, you’re going to miss a lot of fevers." The same philosophy holds true for quantitative waveform capnography.

If you’ve ever dropped off an intubated, post-ROSC patient with an ETCO2 of 40 mm Hg at a ventilatory rate of 10 breaths/minute, only to see the ED staff immediately double your ventilatory rate under the erroneous assumption that all post-arrest patients are acidotic, or had an ED nurse look at you like you’ve sprouted a second head when you say you didn’t administer a bronchodilator to a known asthma patient because both your capnograph and your stethoscope confirmed that there was no evidence of bronchospasm, then you know that not every ED staffer understands capnography like we do.īut if you’ll follow these capnography documentation and handoff tips, you’ll paint a much clearer picture of the patient’s condition, and do a better job of explaining how capnography findings relate to that condition. So when you hand off your patient to the accepting ICU staff at the trauma center, how do you justify your decision to adjust the vent settings to a more appropriate rate of 12 breaths/minute? A quick perusal of the patient’s chart reveals arterial blood gases drawn five minutes after the patient was intubated an hour ago, and none taken since. Your patient’s hemodynamics are within acceptable parameters, and he seems to be tolerating the ventilator well, but when you attach your transport ventilator and end-tidal capnography adaptor, you see what you had suspected your patient’s ETCO2 is only 20 mm Hg, well below physiologic norms. Vent settings are assist/control mode, FiO2 of 40 percent, tidal volume of 650 mL, PEEP of 5.0 cm H20, and ventilatory rate of 16. Your patient has a subarachnoid hemorrhage, and was intubated in the ED and placed on a propofol infusion for sedation. You’re picking up a patient in the ED, for a critical care transfer to the ICU at a Level I trauma center an hour away.


 0 kommentar(er)
0 kommentar(er)
